[table width =”100%” style =”” responsive =”true”]
[table_head]
[th_column]How is medical waste disposed of?[/th_column]
[/table_head]
[table_body]
[table_row]
[row_column]
How to Dispose of Medical Waste?
Medical waste is disposed of by first making it safe through a sterilization process. Waste that cannot be recycled, like gauze or needles, still needs to be made sanitary and non-hazardous before it can be disposed of. This process is usually done by using an autoclave. A medical autoclave is a device that uses steam to sterilize equipment and other objects. This means that all bacteria, viruses, fungi, and spores are inactivated by using temperature’s so high, that no bacteria can survive and thus the items are deemed safe for recycling or disposal.[/row_column]
[/table_row]
[/table_body]
[/table]
Autoclaving is often used to sterilize medical waste prior to disposal in the standard municipal solid waste streams. This application has become more common as an alternative to incineration due to environmental and health concerns raised because of the combustion “by-products” emitted by incinerators, especially from the small units which were commonly operated at individual hospitals. Incineration or a similar thermal oxidation process is still generally mandated for pathological waste and other very toxic and/or infectious medical waste.
Medical waste is generated from medical and biological activities, such as the diagnosis, prevention, or treatment of diseases. Producers (or generators) of medical waste include veterinary clinics, health clinics, funeral homes, nursing homes, hospitals, medical research laboratories, physician offices, dentist and home health care.
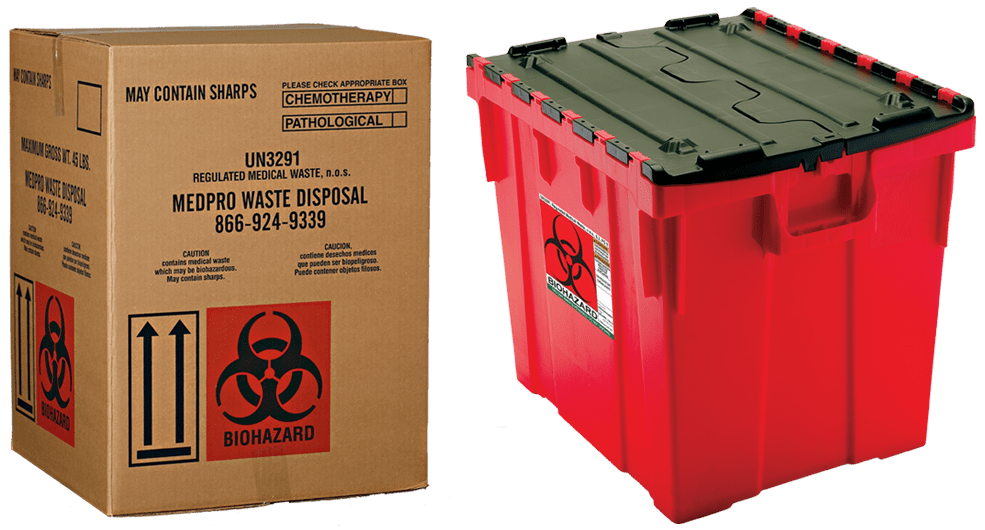
Generally Medical waste is classified as; healthcare waste that that may be contaminated by blood, body fluids or other potentially infectious materials and has the potential (left untreated) to harm humans, animals, or the environment. This type of waste is often referred to as regulated medical waste, biomedical waste or simply medical waste. The classification of medical waste can vary from state to state be sure to check your local laws governing medical waste.
In 1988 the U.S. federal government passed the Medical Waste Tracking Act which set the standards for governmental regulation of medical waste. This was enacted after a 30-mile garbage slick composed primarily of medical and household waste prompted closures of numerous New York and New Jersey beaches for extended periods of time. This act expired in 1991 and since, medical waste is primarily regulated by state environmental and health departments.
There are other federal agencies that have regulations regarding medical waste. These agencies include CDC (centers for disease control), OSHA (Occupational Safety and Health Administration), the FDA (U.S. Food and Drug Administration) and other potential federal government agencies (DOT for example).
OSHA is one example of a federal agency that has regulations regarding medical waste; the OSHA code of federal regulations 29 CFR 1910.1030 has many parts to it. We have highlighted some of the bullet points below but you should visit this page on the U.S. Department of Labor to view the full CFR.
- Exposure Control Plan – Each employer having an employee(s) with occupational exposure as defined by CFR 29 1910.1030 shall establish a written Exposure Control Plan designed to eliminate or minimize employee exposure.
- Methods of Compliance – Universal precautions shall be observed to prevent contact with blood or other potentially infectious materials. When differentiation between body fluid types is difficult or impossible, all body fluids shall be considered potentially infectious materials.
- Personal Protective Equipment – When there is occupational exposure, the employer shall provide, at no cost to the employee, appropriate personal protective equipment such as, but not limited to, gloves, gowns, laboratory coats, face shields or masks and eye protection, and mouthpieces, resuscitation bags, pocket masks, or other ventilation devices.
- Training – The employer shall train each employee with occupational exposure in accordance with the requirements of CFR 29 1910.1030. Such training must be provided at no cost to the employee and during working hours. The employer shall institute a training program and ensure employee participation in the program.
- Vaccination – The employer shall make available the hepatitis B vaccine and vaccination series to all employees who have occupational exposure, and post-exposure evaluation and follow-up to all employees who have had an exposure incident.