The definition of SBAR comes from its acronym, “Situation, Background, Assessment, Recommendations.” It’s the best practice for nurses to communicate info to physicians and other health professionals.
In this article, you’ll find:
- An explanation of how and when to use this standardized communication tool.
- Several hypothetical SBAR use case examples.
- A convenient SBAR template PDF download form for use in any healthcare communication situation.
What is SBAR?
SBAR is a standard way to communicate medical info. It improves accuracy and cuts down on dangerous errors.
SBAR is an acronym. The meaning of SBAR is as follows:
- Situation
- Background
- Assessment
- Recommendations
The above terms represent the four key facts that must be conveyed.
SBAR is a standardized, safe, simple way for nurses and doctors to share patient information in a sharp, clear way.
Why Use SBAR?
In a word: accuracy.
SBAR is endorsed by the Joint Commission as the best practice for communication for physicians and nurses.
The Joint Commission endorses SBAR as an easy-to-use tool to improve communication. According to the Commission, the tool lets nurses send a complete message to doctors concerning a patient’s condition.
Because information is given in a standardized way, there’s less room for human error. This greatly improves accuracy.
Find Out How Much You Can Save Instantly.
Try our online savings calculator.
When to Use SBAR
Use SBAR to communicate any urgent or nonurgent patient information to other healthcare professionals like doctors or therapists. Include:
- Conversations with physicians, physical therapists, or other professionals.
- In-person discussions and phone calls.
- Shift change or handoff communications.
- When resolving a patient issue.
- Daily safety briefings.
- When you’re escalating a concern.
- When calling an emergency response team
How to Use SBAR
Whether you’re using SBAR in written or oral communication, take the time to organize your thinking as follows:
- Situation. Create a brief statement of the problem. The word “brief” here is key. A big part of SBAR is removing irrelevant information. Make sure to identify yourself, your unit, and give the patient’s name.
- Background. Give a concise overview of the situation. This may include diagnoses, medical history, dates, medication info, or names of physicians involved. Basically, anything that’s relevant.
- Assessment. Sum up what you think is going on. Consider results of any lab tests. If you can’t create a clear assessment, just say that.
- Recommendations. Clearly state what you’re requesting. Be specific about suggested action and time frame. In verbal communication, repeat back any order for greatest accuracy. Making a recommendation can be as simple as saying, “I’d like you to check on this patient.”
SBAR Guidelines
SBAR doesn’t happen in a vacuum. Make sure to do the following:
- Carefully think through the problem and your approach before calling, speaking to, or writing to a physician.
- Think what information the physician will require, and have it handy. This might include lab results, medication records, or a patient’s chart.
- Organize your facts according to the SBAR checklist. Be as brief as possible, while including all the relevant data.
- If you’re nervous about making a recommendation, you can simply state that you’re concerned about the situation. Alternately, make a suggestion as a simple starting point for a discussion. Don’t worry that your suggestion will be followed blindly.
SBAR Templates
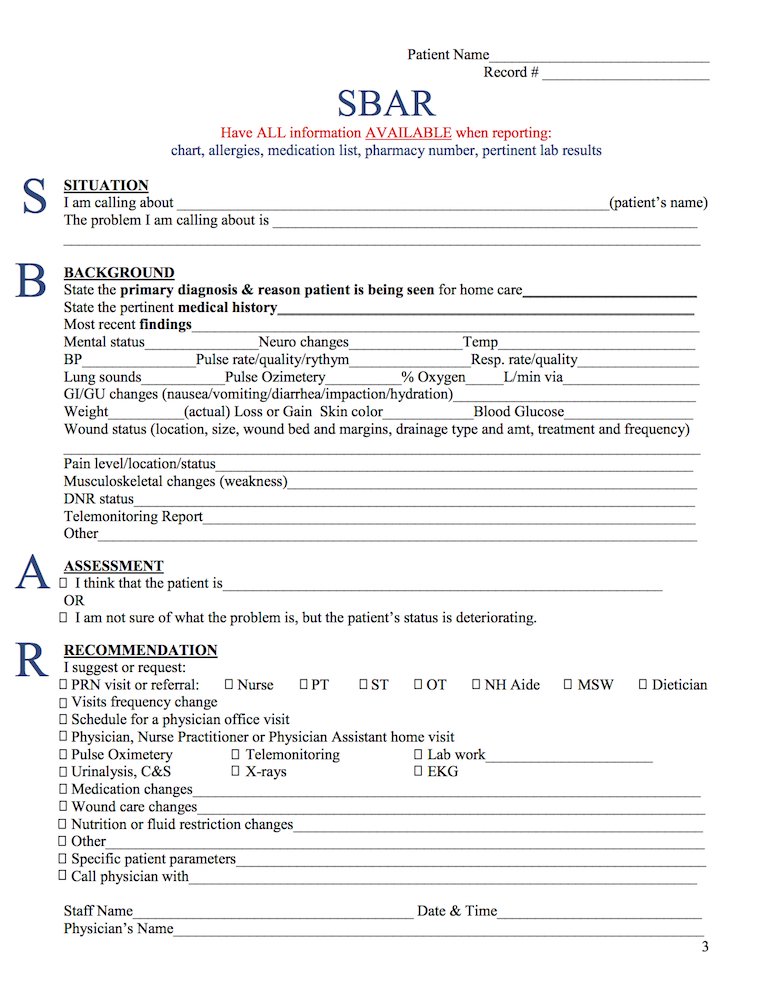
The SBAR PDF shown here comes from Missouri.gov and is available free of copyright. It covers all pertinent information, including Situation, Background, Assessment, and Recommendation. It’s a simple, one-page SBAR form. You can download it for use in actual communications or just use it as an SBAR worksheet.
There’s a more complete SBAR worksheet here. This PDF is offered for use by the State of Indiana.
Alternately, here are a couple of condition-specific SBAR PDFs from the US Government’s Agency for Healthcare Research and Quality:
- UTI SBAR PDF for nursing home use. (Specifically for Urinary Tract Infections, courtesy of AHRQ.gov)
- LRI SBAR PDF for nursing home use. (Specifically for Lower Respiratory Infections, courtesy of AHRQ.gov)
Who Should Use SBAR?
According to AHRQ, SBAR should be used by:
- Nurses communicating to physicians
- Nursing assistants communicating with nurses.
- Physicians to other physicians
- Residents to attending physicians
- Nurses to other nurses
- Nurses to technicians
- Pharmacy to nurses and/or physicians
- Administrators to physicians
Though SBAR is primarily used by Nurses, there’s no reason why doctors shouldn’t use it when communicating with each other. For example, a GP can effectively use the tool to request advice from a specialist on a certain patient’s case.
Where Does SBAR Come From?
SBAR was developed by the U.S. military. Specifically, it was created to improve communication in the use of nuclear submarines. It spread from there into the aviation industry, and then into healthcare.
Kaiser Permanente adapted the tool for its rapid response teams in 2002, as a method of investigating patient safety. The company had identified communication problems arising from personal differences in communication styles. SBAR was found to flatten out those differences, allowing smooth, standardized communication that got the facts from person to person with minimal mistakes.
SBAR became the communication standard for nurses when the Joint Commission endorsed it in 2013.
Examples of SBAR in Use
Here are three SBAR scenarios to make it easier to use this valuable tool more effectively. Two are SBAR examples in nursing settings while one is a medical order example.
Note that SBAR can be used very formally, but it can also be used quite informally. The key is to go through the thought process so all relevant details are included, and all superfluous details are left out.
SBAR Scenario #1
- Situation: I’m nurse Karen Smith from XYZ Medical, calling about Mr. F. His temperature was elevated throughout the night. He is now shivering.
- Background: Mr. F. has a history of severe bladder infections and an indwelling catheter. Her temperature is now 101 degrees and his urine is foul-smelling and cloudy. In the past, a high temperature has signalled infection. His catheter was changed two weeks ago. He took Tylenol every four hours through the night. He presents as increasingly more confused.
- Assessment: Mr. F seems to have a UTI.
- Recommendation: I’d like to get a urine sample order for sensitivity and culture. Based on the results, I’d like to suggest an antibiotic. In the meantime, I suggest encouraging Mr. F. to drink more fluids.
SBAR Scenario #2
- Situation: I’m nurse Bill Jones from XYZ Home Care. I’m calling about Mrs. P. Her weight, respirations, and blood pressure are all elevated.
- Background: Mrs. P. is a 75-year-old patient. She has a diagnosis of HTN and CHF. Her BP has increased to 190/92 and her respirations to 25. SOB when ambulating 7 feet. Previously SOB at 25 feet. Weight increased 7 lbs in 5 days. Crackles in posterior bilateral lower bases x 1/4 lung field. Compliant with both medications and low sodium diet. One exception is a very salty dinner yesterday.
- Assessment: Mrs. P. has fluid retention, possibly made worse by the salty dinner.
- Recommendation: I’d like to give Mrs. P. a dose of IV Lasix. Then I’d like to continue with her daily a.m. Lasix dose. I’d like to have her husband measure urine output for one day to assess dieresis. I’d like an order to assess urine output and respiratory status. I’d also like you to make further recommendations as I’m concerned about her SOB.
SBAR Scenario #3
- Situation: Hi Dr. C, this is Sharon in CT. I’ve got an order for patient L. for a PE study. I’d like to clarify the order because he has elevated creatinine.
- Background: Patient L. came in with difficulty breathing and right-side chest pain.
- Assessment: Patient L.’s creatinine level is 3.1. That’s far above our cutoff level for a PE study.
- Recommendation: I think we should change the PE study order to a VQ scan order.
SBAR Critical Words
The goal with SBAR is to get someone to take action. That means the recommendation must be taken seriously.
Using “critical” language increases the urgency of your suggestion. Use words like “now,” and “immediately” when the situation is urgent. Here are some other critical words to use in SBAR communication:
- Must
- Now
- Need
- Critical
- Immediately
- Important
- Priority
- Quickly
- At Once
- Requires
- Acute
- Instantly
- Vital
- Imperative
- Urgent
- Crucial
- Essential
SBAR Videos
The two videos in this section help with understanding SBAR communication.
The first SBAR video is from the Nurse Mendoza show. It’s an informative, 3-minute explanation of what SBAR is and how to use it. It covers patient handoffs in terms of vitals (situation), patient background, assessment, and recommendation. There’s an emphasis on how to perform a patient assessment.
The next video is from Ashley Adkins, RN. It’s a short SBAR video that shows exactly how to give an SBAR from a nurse to a doctor. It does a really good job of giving examples that’ll help you know what not to include, which is a vital part of SBAR.
Life Without SBAR
Before SBAR, communication often failed in the medical world for several reasons. Sometimes a nurse would simply fail to get the attention of a doctor or other healthcare professional. At other times, the nurse wouldn’t adequately get across her/his level of concern.
At still other times, a nurse wouldn’t communicate the real problem, or would fail to explain the desired action.
What SBAR Does
Studies have shown that in healthcare situations, critical information is often left out of interaction between professionals. These omissions reduce patient safety.
The introduction of SBAR has been shown to enhance patient outcomes. It makes nurses more effective. It also creates higher patient and family satisfaction scores, and makes reports more relevant and concise.
SBAR has improved communication between nurses and doctors. More importantly, it has had a dramatic effect on overall patient health. It has led to less hospitalizations, shorter hospitalizations, and less patient death.
The Limits of SBAR
SBAR doesn’t help in every situation. The tool’s main problems occur when:
- Users don’t understand the correct way to use SBAR.
- Nurses and other users may feel insecure about completing the “Recommendation” part of the tool.
- SBAR may run into HIPAA issues. Problems can occur when discussing patient information that gets overheard by others.
Conclusion
SBAR is an easy-to-use method for improving accuracy in medical communication. It works best for nurse/physician interaction, either verbally or in written form. It’s a standardized communication method endorsed by the Joint Commission to increase patient safety.
The SBAR PDF form in this article gives a good starting point for communicating patient information in a standardized, effective way.
See how much your facility could save on sharps container disposal with MedPro Waste Disposal by trying out the savings calculator below.