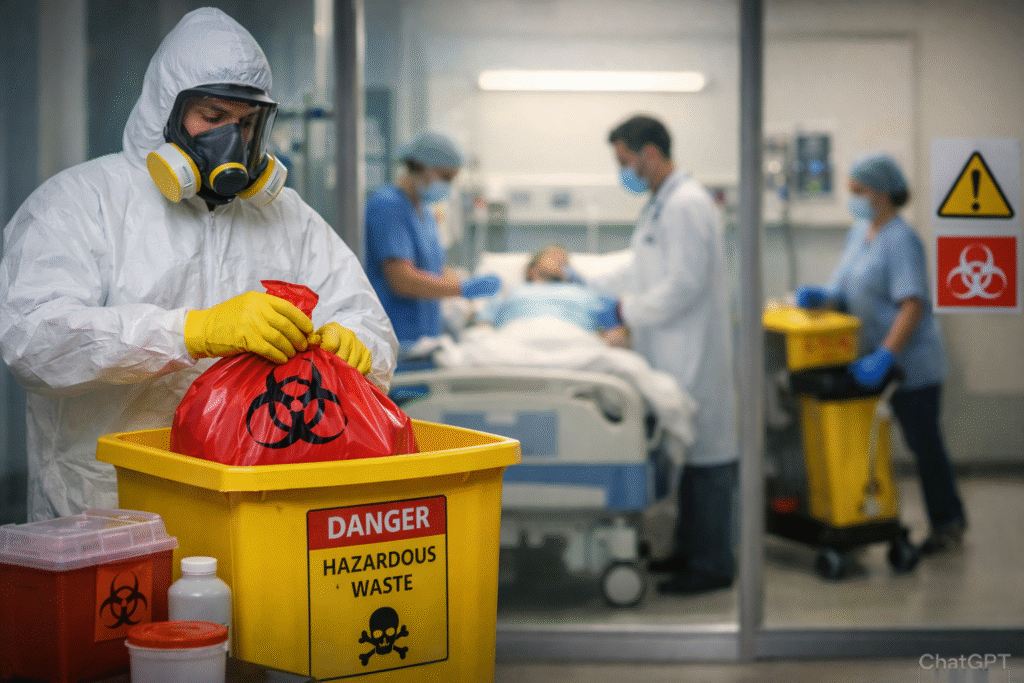
Proper hazardous waste handling in hospitals directly reduces staff exposure to infectious materials, prevents regulatory violations, and minimizes contamination risks that can lead to patient infections. Healthcare facilities that implement comprehensive hospital hazardous waste management protocols experience fewer workplace injuries, lower liability costs, and maintain compliance with OSHA, EPA, and state regulations. Effective healthcare hazardous waste safety practices protect both clinical staff and patients while ensuring environmental responsibility.
Understanding Hazardous Waste Categories in Hospital Settings
Hospitals generate multiple hazardous waste streams that require specific handling protocols to maintain safety standards.
Types of Hazardous Waste in Healthcare Facilities
Medical hazardous waste disposal encompasses several distinct categories. Infectious waste includes blood-soaked materials, contaminated PPE, and culture dishes that can transmit diseases. Sharps waste consists of needles, scalpels, and lancets that pose puncture and infection risks. Chemical waste includes disinfectants, solvents, and laboratory reagents that can cause burns or toxic exposure.
Pharmaceutical waste requires separate handling, particularly controlled substances and chemotherapy agents. Trace chemotherapy waste contains minimal residual agents (less than 3% of original volume), while bulk chemotherapy waste exceeds these thresholds and demands specialized disposal methods.
Regulatory Framework Governing Hospital Waste
Hospital waste safety practices must comply with multiple regulatory bodies. OSHA’s Bloodborne Pathogens Standard (29 CFR 1910.1030) mandates exposure control plans and employee training. The EPA enforces the Resource Conservation and Recovery Act (RCRA), which classifies hazardous waste by ignitability, corrosivity, reactivity, and toxicity characteristics.
State regulations often impose additional requirements beyond federal standards. Hospitals must maintain current knowledge of jurisdiction-specific rules regarding storage duration limits, container specifications, and transportation protocols. Non-compliance results in substantial fines, service refusal by waste transporters, and potential facility shutdowns.
Implementing Effective Waste Segregation Systems
Proper segregation at the point of generation forms the foundation of safe hazardous waste handling in hospitals.
Color-Coded Container Systems
Standardized color coding prevents dangerous waste mixing. Red containers hold infectious waste and materials saturated with blood or body fluids. Yellow containers store trace chemotherapy waste and contaminated PPE from oncology departments. Black containers with hazardous waste labels contain chemical waste that requires specialized treatment.
Sharps containers must be puncture-resistant, leak-proof, and clearly labeled. These containers should be placed within arm’s reach of procedures generating sharps waste to prevent unsafe disposal attempts. Container fill lines must not be exceeded, as overfilled containers create puncture risks during handling and transportation.
Staff Training and Compliance Protocols
Comprehensive training ensures all hospital personnel understand waste classification and proper disposal procedures. Initial training should occur before employees handle any hazardous materials, with annual refresher courses maintaining competency.
Training programs must cover waste stream identification, proper container selection, labeling requirements, and emergency response procedures for spills or exposures. Documentation of training completion satisfies OSHA requirements and provides liability protection during regulatory inspections.
Safe Storage and Transportation Practices
Temporary storage areas within hospitals require specific design features to prevent environmental contamination and staff exposure.
Secure Storage Requirements
Designated storage areas must be clearly marked, restricted to authorized personnel, and equipped with proper ventilation. Storage duration limits vary by state but typically range from 30 to 90 days for regulated medical waste. Temperature-controlled storage prevents decomposition and odor issues in warmer climates.
Secondary containment systems protect against container leaks. Impermeable flooring and spill containment berms prevent hazardous materials from entering drainage systems. Storage areas should maintain separation between incompatible waste types, particularly chemical wastes that could react dangerously if mixed.
Transportation and Chain of Custody
Licensed waste transporters must maintain proper credentials and carry comprehensive liability insurance. Transportation vehicles require specific features including locked compartments, leak-resistant designs, and clearly visible biohazard symbols.
Waste manifests document the chain of custody from generation through final disposal. These documents include waste classification, quantity, generator information, transporter details, and treatment facility confirmation. Hospitals retain manifests for three years minimum to demonstrate regulatory compliance during inspections.
Reducing Exposure Risks Through Proper Handling
Direct contact with hazardous waste creates multiple health risks that proper protocols effectively minimize.
Personal Protective Equipment Standards
Healthcare hazardous waste safety requires appropriate PPE for all handling activities. Gloves must be puncture-resistant when handling sharps containers and chemical-resistant when managing pharmaceutical or chemical waste. Face shields protect against splashes during waste bag closure or container movement.
Disposable gowns prevent contamination of personal clothing and skin exposure. Closed-toe shoes with slip-resistant soles reduce injury risks in storage areas where spills may occur. All PPE must be removed immediately after waste handling and disposed of as contaminated material.
Spill Response and Decontamination
Immediate spill response prevents exposure escalation. Spill kits should be readily accessible in all areas generating hazardous waste. Kit contents include absorbent materials, disinfectants, PPE, and clearly marked disposal bags for contaminated cleanup materials.
Small spills (less than 10 milliliters) can typically be managed by trained staff using facility protocols. Larger spills or those involving highly infectious materials require professional response teams. Affected areas must be decontaminated using EPA-registered disinfectants at proper concentrations and contact times before resuming normal operations.
Frequently Asked Questions
What qualifies as hazardous waste in hospitals?
Hazardous waste in hospitals includes infectious materials (blood, body fluids, contaminated items), sharps (needles, scalpels), chemical waste (disinfectants, laboratory reagents), pharmaceutical waste (expired medications, chemotherapy agents), and radioactive materials. Each category requires specific handling and disposal methods according to OSHA, EPA, and state regulations.
How often should hospital hazardous waste be collected?
Collection frequency depends on waste generation volume and state regulations. High-volume facilities may require daily or twice-weekly pickups, while smaller hospitals might schedule weekly collections. Storage duration typically cannot exceed 30-90 days depending on jurisdiction. Regular collection prevents accumulation that increases contamination and exposure risks.
Who is responsible for hospital hazardous waste compliance?
The waste generator (hospital) maintains responsibility until a licensed transporter takes custody. Hospital administration must ensure proper segregation, storage, and documentation. Environmental health and safety departments typically oversee compliance programs, while all staff members who generate or handle waste share responsibility for following established protocols.
What are the penalties for improper hazardous waste handling?
Penalties vary by violation severity and jurisdiction. OSHA fines for bloodborne pathogen standard violations range from $7,000 to $70,000 per violation. EPA RCRA violations can result in fines up to $37,500 per day per violation. State agencies may impose additional penalties. Serious violations can lead to facility closure, criminal charges, and civil lawsuits.
How can hospitals reduce hazardous waste generation?
Hospitals can reduce waste through product substitution (using less hazardous alternatives), purchasing only necessary quantities to minimize expired pharmaceuticals, implementing reusable sharps containers where appropriate, and training staff on proper waste segregation to prevent non-hazardous materials from contaminating hazardous waste streams.
What training is required for staff handling hazardous waste?
OSHA requires initial training before employees handle hazardous materials and annual refresher training thereafter. Training must cover waste identification, proper handling procedures, PPE use, emergency response, and exposure prevention. Documentation of training completion must be maintained and available during regulatory inspections.

Ben Brenner is a founding partner at MedPro Disposal with over 9 years of hands-on experience in healthcare operations and medical waste management. He works closely with healthcare facilities to ensure OSHA-compliant sharps disposal, regulatory adherence, and safe waste handling practices. Ben contributes industry-backed insights based on real operational experience in the healthcare sector.